What is a Digital Clinical Safety Management System?
A digital clinical safety management system is a structured way of managing the risks involved in using digital tools in your practice.
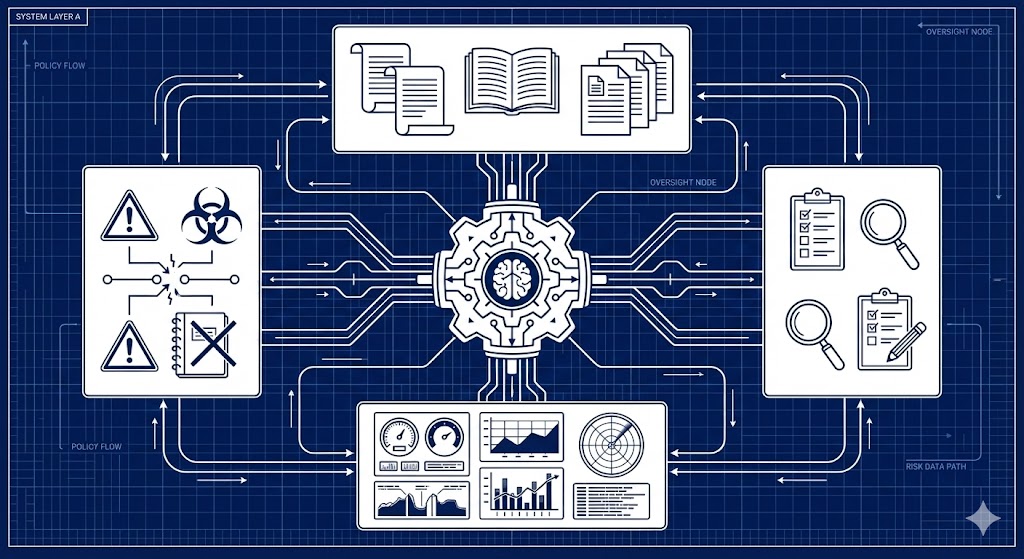
It is not software you can buy. It is not a complicated certification scheme. It is a set of written-down principles (policies) and processes (standard operating procedures) that describe how you identify risks, control them, and keep track of what you are doing.
At its core, a management system answers three questions:
- What digital systems do we use? (your inventory)
- How do we make sure they are safe? (your policies and procedures)
- How do we prove we are doing it? (your documentation and records)
If you can answer those three questions with written evidence, you have a management system.
Why You Need One
DCB0160 requires that organisations deploying digital health systems manage clinical risk systematically. A management system is how you demonstrate that you are meeting this obligation.
Without a management system, you have no consistent way to:
- Know which digital tools are in use across your practice
- Assess whether those tools are safe in your environment
- Control risks when systems change or new tools are introduced
- Learn from incidents and near misses
- Provide evidence to regulators, commissioners, or auditors
A management system does not guarantee perfect safety—nothing does—but it provides a structured approach to managing risk and a clear audit trail showing you are meeting your legal obligations.
Core Components of a Management System
Every clinical safety management system has the same basic building blocks:
1. Clinical Safety Policy
A short document (typically 2-4 pages) that sets out your organisation's commitment to managing clinical risk. It states:
- That you will comply with DCB0160
- Who your Clinical Safety Officer is and what authority they have
- How risks will be identified, assessed, and controlled
- How incidents will be reported and investigated
- How often the policy will be reviewed
The policy is signed by your accountable officer and CSO. It provides the mandate for everything else you do.
2. Standard Operating Procedures (SOPs)
Practical, step-by-step instructions for how you actually do the work. These might cover:
- How to assess a new digital tool before deployment
- How to review supplier DCB0129 documentation
- How to log and investigate incidents
- How to approve system changes or updates
- How to maintain your hazard log
SOPs do not need to be long or complicated. A good SOP is short, clear, and describes exactly what someone needs to do and in what order.
3. System Inventory
A list (often a spreadsheet) of every digital tool that interacts with patient care or clinical workflows. This includes:
- Your electronic patient record (EPR)
- Online consultation platforms
- Patient messaging apps
- Prescribing tools
- Clinical decision support tools
- AI-assisted triage, scribing, or diagnostic tools
- Remote monitoring platforms
- Appointment booking systems (if used for clinical triage)
For each system, you record what it does, who the supplier is, when it was deployed, and whether a safety assessment has been completed.
4. Clinical Safety Assessments
For each system in your inventory, you need a documented assessment showing:
- What hazards have been identified
- What the risks are (likelihood and severity)
- What controls are in place to reduce risk
- What residual risks remain and why they are acceptable
These assessments follow the DCB0160 process and are recorded in Clinical Safety Case Reports and Hazard Logs.
5. Incident Records and Learning
Documentation of:
- Safety incidents and near misses
- Investigations into what went wrong
- Actions taken to prevent recurrence
- Updates to hazard logs and controls
The management system ensures that incidents are not just logged and forgotten—they are analysed and used to improve safety.
6. Ongoing Monitoring and Review
Regular activities to ensure the system stays current:
- Safety reviews (monthly or quarterly)
- Updates to the inventory when systems are added or removed
- Reassessments when systems change significantly
- Annual policy reviews
A management system is not a one-time exercise. It is an ongoing process embedded in how your practice operates.
What a Management System is NOT
It is worth being clear about what a management system is not:
- Not inherently software: You do not need to buy a tool or platform. A management system can be maintained using documents, spreadsheets, and folders. That said, software tools can help streamline the work—Protect Clinical, for example, provides a digital clinical safety governance platform designed specifically to help GP practices manage DCB0160 compliance more easily.
- Not a certificate: There is no external body that "certifies" your management system. Compliance is demonstrated through evidence, not badges.
- Not perfect: A management system does not eliminate all risk. It provides a structured way to identify, assess, and control risks—but risks remain.
- Not static: A management system evolves as your practice changes, new systems are deployed, and lessons are learned from incidents.
How a Management System Relates to Other Frameworks
Your clinical safety management system connects with other governance frameworks you may already use:
- Data Security and Protection Toolkit (DSPT): Many clinical safety processes (such as incident management, change control, and staff training) overlap with DSPT requirements.
- Care Quality Commission (CQC): Your management system provides evidence for the Safe and Well-led domains.
- Digital Technology Assessment Criteria (DTAC): Evidence you gather for clinical safety can support DTAC assessments.
A well-designed management system integrates with these frameworks rather than duplicating them.
Getting Help: Shared Models and Collaboration
You do not have to build everything from scratch. Many Primary Care Networks (PCNs), federations, and Integrated Care Boards (ICBs) provide:
- Template policies and SOPs
- Shared hazard logs and risk assessment templates
- Peer support networks for Clinical Safety Officers
- Shared CSO services across multiple practices
If you are part of a PCN or federation, ask whether shared resources or support are available. Clinical safety is an area where collaboration makes sense—most practices face the same risks and can learn from each other.
Next Steps: Building Your Management System
Now you understand what a digital clinical safety management system is and what components it includes, you are ready to build one for your practice.
Step-by-step guidance on how to create your management system from scratch—including how to prioritise which systems to assess first, how to write policies and SOPs, and how to maintain your system over time—is available in: How to Build a Clinical Safety Management System from Scratch.
Resources to Bookmark
- DCB0160 – Clinical Risk Management Standard (NHS England)
- What is a Clinical Safety Officer? – Understand the role responsible for your management system
- A Simple Guide to DCB0160 – The standard your management system implements
Key Takeaways
A digital clinical safety management system is a structured framework for managing the risks of digital health technology. It consists of policies that set out your principles, procedures that describe how you do the work, and documentation that provides evidence of what you have done.
The system is not complicated or expensive. It is simply a way of writing down what you do, how you do it, and what you have learned. It provides the structure needed to comply with DCB0160 and the audit trail to demonstrate compliance to regulators and commissioners.
Understanding what a management system is and why you need one is the first step. The next step is building one for your practice.