Why You Need a Clinical Safety Officer
DCB0160 requires every organisation deploying health IT systems to appoint a Clinical Safety Officer (CSO). This is not optional—it is a legal requirement under the Health and Social Care Act 2012.
The CSO is responsible for overseeing clinical risk management across all your digital systems. They assess whether new tools are safe to deploy, review system changes, investigate incidents, and ensure your practice meets its DCB0160 obligations.
If you have not already read it, start with What is a Clinical Safety Officer? to understand the role's qualifications, responsibilities, and legal requirements.
This guide explains how to set up the CSO role in your practice without hiring new staff.
Who Should Be Your CSO?
The CSO must be a registered healthcare professional. Typically, this means:
- A GP partner or salaried GP
- An advanced nurse practitioner
- A pharmacist with clinical involvement
- Another registered clinician with relevant experience
Choose someone who has:
- Senior standing in the practice: The CSO needs authority to challenge decisions and stop deployments if safety concerns arise. A junior member of staff will struggle to exercise this authority.
- Confidence with digital systems: They do not need to be a technical expert, but they should be comfortable using digital tools and understanding how they fit into clinical workflows.
- Communication skills: The CSO must work across the practice—clinicians, reception staff, practice managers, and external suppliers. Clear communication is essential.
- Partnership support: The CSO's decisions on clinical safety must be respected, even when they conflict with operational or financial pressures. Ensure the partnership understands and supports this.
In most GP practices, a GP partner takes on the CSO role. This gives them the authority and standing needed to make difficult decisions.
How Much Time Does the CSO Need?
The time commitment depends on what is happening in the practice:
During Active Change Periods
When you are deploying new systems, conducting assessments, or responding to incidents, the CSO will need approximately 0.1 Whole Time Equivalent (half a day per week).
This time is used for:
- Reviewing supplier DCB0129 documentation
- Conducting risk assessments for new systems
- Approving system changes and updates
- Investigating incidents
- Updating hazard logs and safety case reports
During Steady State
When no major changes are happening, the CSO's workload reduces to approximately 1-2 hours per week.
This time is used for:
- Reviewing incident logs
- Attending monthly or quarterly safety reviews
- Approving routine system updates
- Responding to supplier safety notifications
Protect the Time
The CSO's time must be protected. If it is not built into job plans or rotas, it will be squeezed out by clinical pressures.
Record the CSO's allocated time explicitly. For a GP partner, this might be a protected half-session per week. For a salaried GP or nurse, it should be part of their job description and contracted hours.
What Support Does the CSO Need?
The CSO should not be working alone. They need administrative and governance support from the wider practice team.
Practice Manager or Digital Lead
The practice manager (or a designated digital lead) should provide:
- Documentation management: Maintain the safety file, hazard logs, and safety case reports
- Meeting logistics: Schedule safety reviews, coordinate with suppliers, manage the safety log
- Governance integration: Ensure clinical safety is a standing item in practice meetings and governance structures
This administrative support is critical. Without it, the CSO becomes overwhelmed by paperwork and cannot focus on risk assessment.
Shared Templates and Resources
Do not start from scratch. Use templates for:
- Clinical safety policies
- Standard operating procedures (SOPs)
- Hazard logs
- Risk assessment matrices
- Safety case reports
Many Primary Care Networks (PCNs), federations, and Integrated Care Boards (ICBs) provide shared templates. Your CSO should connect with other CSOs in the area to share resources and learn from their experience.
Peer Support Network
Clinical safety can feel isolating if the CSO is the only person in the practice with this responsibility. Connect with other CSOs through:
- PCN safety forums
- ICB peer networks
- Regional CSO groups
These networks provide peer support, shared learning, and cover during leave.
The Importance of Training
The CSO must complete accredited clinical safety training. This is not optional—DCB0160 requires that the CSO is "suitably qualified."
The most widely recognised training is the NHS England Clinical Safety Officer course (a two-day course covering DCB0129 and DCB0160 in depth). Other accredited providers include the Professional Record Standards Body (PRSB) and Ethos.
What If You Cannot Get Training Immediately?
If you are starting from zero and cannot access training immediately, you have two options:
Option 1: Appoint an interim CSO and log the risk
Appoint a senior clinician as interim CSO, document this as a risk on your practice risk register, and create a plan to get them trained within 6-12 months. This is not full compliance, but it demonstrates you are working towards compliance rather than ignoring the requirement.
Option 2: Use a shared CSO service
Some PCNs and federations provide shared CSO services where a trained CSO covers multiple practices. This can be a good interim solution while you build internal capacity.
For more detail on this pragmatic approach, see How to Build a Clinical Safety Management System from Scratch.
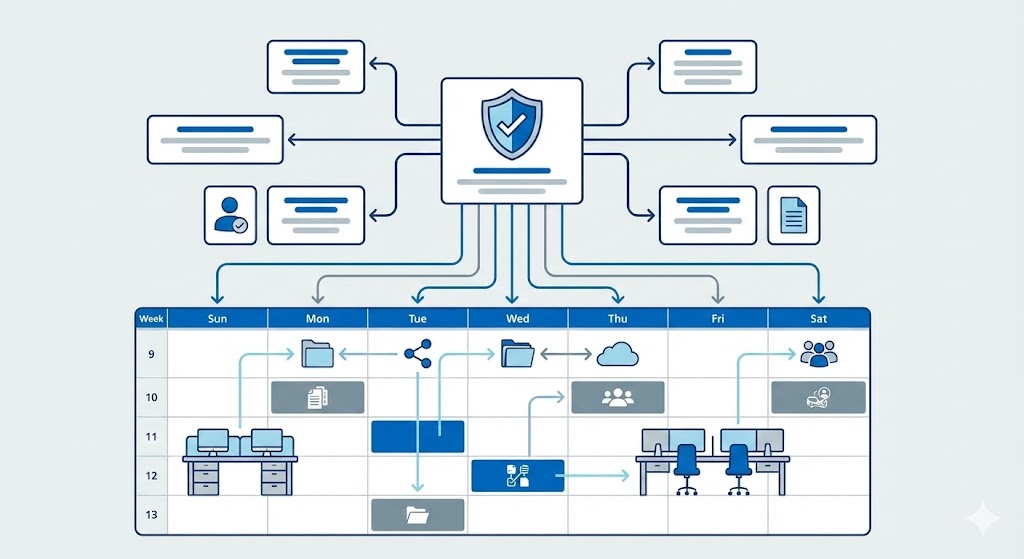
Setting Up the Role: Practical Steps
Step 1: Identify the CSO and Secure Buy-In
Choose a senior clinician and confirm that the partnership supports the role. The CSO must have the authority to make decisions, including the power to pause or stop deployments.
Step 2: Allocate Protected Time
Record the CSO's allocated time in job plans, rotas, or contracts. Make it explicit so it is protected from competing demands.
Step 3: Arrange Training
Book the CSO on an accredited clinical safety training course. If training is not immediately available, document an interim plan.
Step 4: Set Up Supporting Processes
Establish the basic infrastructure the CSO needs:
- A safety file (a folder or shared drive containing policies, SOPs, hazard logs, and safety case reports)
- A safety log for staff to report incidents and concerns
- A process for the CSO to review system changes before they go live
- A monthly or quarterly safety review meeting
Step 5: Integrate with Governance
Add clinical safety as a standing agenda item in:
- Practice meetings
- Safety huddles
- Quality improvement reviews
This ensures clinical safety is embedded in how the practice operates, not treated as a separate compliance exercise.
Step 6: Connect with Peer Support
Identify other CSOs in your PCN, federation, or ICB. Set up regular peer sessions (e.g., quarterly) to share learning, templates, and challenges.
Shared CSO Models
If no single clinician in your practice has capacity to be the CSO, consider a shared model:
PCN Shared CSO
Appoint one CSO across multiple practices in the PCN. The CSO has deputies at each practice who handle day-to-day tasks, with the lead CSO providing oversight, reviewing high-risk assessments, and coordinating shared resources.
This model works well for small practices that do not have the capacity for a dedicated CSO.
Federated CSO Service
Some federations provide a CSO-as-a-service model, where a trained CSO covers multiple practices on a part-time or contracted basis. This can be a good interim solution while practices build internal capability.
Hybrid Model
Appoint a practice-based CSO for routine tasks, with access to a senior CSO at PCN or federation level for complex assessments, escalations, or peer review.
Whichever model you choose, document it clearly in your clinical safety policy and ensure roles and responsibilities are understood.
Common Pitfalls to Avoid
Pitfall 1: Unprotected Time
If the CSO's time is not explicitly protected, it will be squeezed out by clinical pressures. Build it into job plans and rotas from the start.
Pitfall 2: Vague Responsibilities
"You are the CSO" is not enough. Document exactly what the CSO is responsible for, what decisions they can make, and what authority they have.
Pitfall 3: No Administrative Support
Clinicians cannot do clinical risk assessment and manage all the documentation. Provide practice manager or digital lead support for paperwork, scheduling, and governance.
Pitfall 4: Working in Isolation
The CSO should not be the only person who knows about clinical safety. Integrate it into governance, involve the wider team, and connect with peer networks.
Pitfall 5: No Succession Plan
What happens if the CSO leaves, goes on long-term sick leave, or retires? Identify a deputy and ensure knowledge is documented so the role can continue.
Action Checklist
- Identify a senior clinician to act as CSO and secure partnership support
- Allocate protected time (0.1 WTE during active periods, 1-2 hours weekly during steady state)
- Record the CSO's allocated time in job plans or contracts
- Book the CSO on accredited clinical safety training (or document an interim plan)
- Set up a safety file, safety log, and change control process
- Provide practice manager or digital lead support for documentation
- Add clinical safety as a standing item in practice meetings and governance
- Connect with other CSOs in the PCN, federation, or ICB
- Identify a deputy CSO to cover leave and ensure succession planning
Resources to Bookmark
- What is a Clinical Safety Officer? – Understand the role's qualifications and responsibilities
- How to Build a Clinical Safety Management System – Set up the framework the CSO operates within
- NHS England Clinical Safety Officer Training – Book accredited training
- DCB0160 Standard (NHS England)
Key Takeaways
A Clinical Safety Officer can be established without new headcount by allocating protected time, providing administrative support, and embedding the role into existing governance structures.
The CSO must be a senior clinician with authority to make decisions. They need training, protected time (half a day per week during active periods), and support from the practice manager or digital lead.
Shared CSO models across PCNs or federations work well for smaller practices. Connect with peer networks to share learning and avoid working in isolation.
Most importantly, the CSO's authority must be respected. If they say a system is not safe to deploy, that decision is final—even when it conflicts with operational or financial pressures.